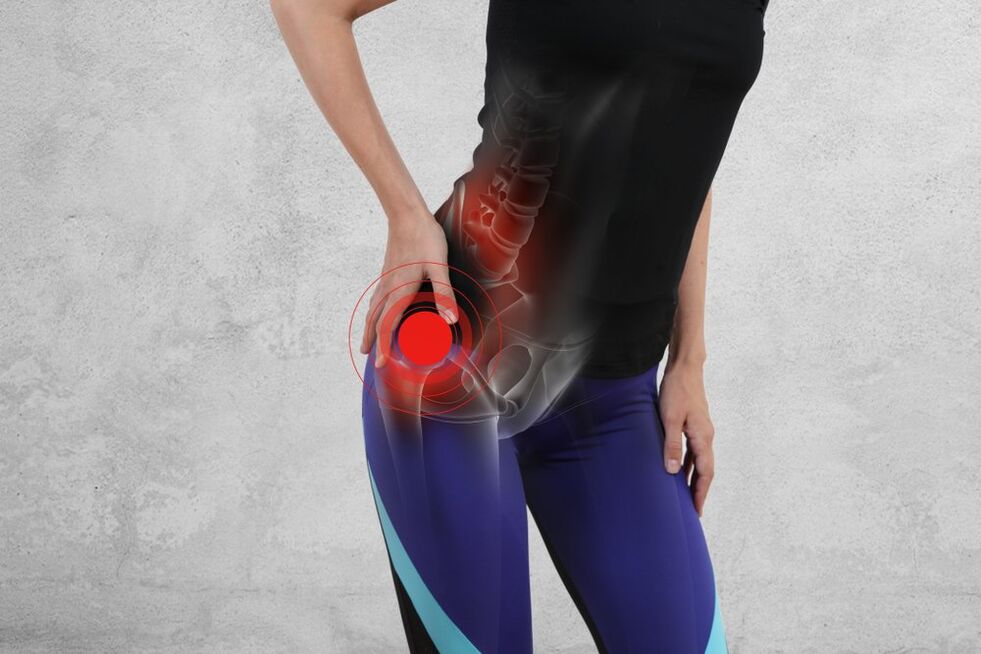
Throughout life, leg joints experience a lot of stress. The hip is a large ball joint that provides the ability to move independently. The appearance of painful sensations, tense movements, limping gait makes a person think about the appearance of pathology.
In recent years, the number of people under the age of 30 who have been diagnosed with osteoarthritis has increased dramatically. This statistic is extremely disappointing as the disease progresses steadily and can lead to serious disability and impairment. To protect yourself from the development of adverse effects, you should immediately start treatment and follow all medical recommendations.
Osteoarthritis of the hip joint causes a lot of inconvenience to its owner. If there is discomfort in the joint area, it is necessary to consult a doctor to confirm the diagnosis and prescribe an effective treatment. Late treatment can cost the patient the ability to walk independently.
what is osteoarthritis
Osteoarthritis is a rheumatologic disease, which is based on degenerative and dystrophic changes in the joints. At the same time, not only the joint surfaces, but also the ligament apparatus and capsule are involved in the pathological process. Most often, the joints of the hands, feet, knees suffer, but the most serious disease is arthrosis of the hip joint. With its development, the risk of developing total disability increases due to severe restrictions in movement.
The basis of articular cartilage is composed of collagen molecules and proteoglycans: they are what give strength and elasticity to the joint, making it resistant to various types of loads. Under the influence of external factors, the amount of collagen and proteoglycans decreases, resulting in depletion and gradual destruction of cartilage tissue. Osteoarthritis develops under the influence of the following factors:
- mechanical injury;
- inflammatory processes in the joints;
- excessive load on the lower limbs;
- obesity;
- age-related body changes (in people over 55);
- menopause (in women);
- malnutrition with protein and calcium deficiency;
- hereditary predisposition;
- operations transferred in the joints.
How is osteoarthritis of the hip joint manifested?

Osteoarthritis develops gradually, so it is quite difficult to detect its initial manifestations. The patient may ignore the symptoms of the disease, mistaking them for fatigue or overwork. Exacerbation of discomfort can occur after an injury. Osteoarthritis of the hip joint is accompanied by the following symptoms:
- Pain in the affected limb. It is dull, painful by nature, constant throughout the day. Unpleasant sensations increase during physical activity (exercise, running or walking), decrease at rest. When the hip joint is affected, the pain radiates to the groin, perineum, and thigh. The joint may also begin to "respond" to changes in weather conditions or atmospheric pressure.
- Atrophic muscle changes. When walking, the patient unconsciously spares the affected limb, resulting in less stress on the muscles of the buttocks and thighs. This is accompanied by their atrophy and decrease in volume. This is especially noticeable with unilateral osteoarthritis.
- The appearance of a crisis during the execution of movements in the joint. This sound resembles the rustling of a plastic bag and becomes louder after a long period of immobility (night sleep). In medicine, this term is called "crepitus". The appearance of a crisis is associated with a violation of joint mobility.
- Increase in the volume of the affected joint. This occurs as a result of the formation on the bone surfaces of the smallest spikes - osteophytes. Such a reaction occurs as a compensatory response to an increased load on the bone surface (thinning the cartilage).
Medical treatment of osteoarthritis
Currently, it is not possible to completely prevent the destruction of cartilage tissue. Therefore, treating osteoarthritis with the help of medications is aimed at reducing pain and slowing down the progression of the disease. Most often, the following groups of drugs are used in therapy:
- Non-narcotic analgesics and mixed-action analgesics. They help reduce pain and are available in tablets or ampoules for intravenous administration.
- Non-steroidal anti-inflammatory drugs in the form of topical ointments or creams are also used to control pain. They are also prescribed if osteoarthritis is accompanied by inflammation of the synovial membrane of the joint.
- Chondroprotectors are drugs that slow the progression of the disease and improve joint function.
Exercise therapy and physical therapy methods

Non-pharmacological agents are also widely used to combat the disease. Doctors prescribe exercise therapy to patients to strengthen muscles and prevent joint immobility from developing. The nature of the exercises and the frequency of their execution are determined individually for each case. Osteoarthritis treatment also includes physical therapy procedures such as:
- Transcutaneous electrical nerve stimulation;
- acupuncture;
- magnetic therapy;
- electrophoresis with analgesics;
- laser therapy;
- massage.
To reduce the load on the affected limb, the patient is also recommended to use canes or a walker. It will be helpful to wear a hip orthosis, a special device that helps restore leg function and prevent further damage to the joint.
Surgery
Endoprosthesis is prescribed in the event that conservative methods of treating arthrosis of the hip joint are ineffective. The aim of surgery is to eliminate the pain syndrome and restore motor function to the limb. The procedure is performed under general anesthesia in a specialized hospital, after which the patient will have a long rehabilitation. The most favorable working prognosis is in patients aged 40 to 75 years with a body weight of up to 70 kg: the probability of endoprosthesis rejection is minimized in them, which makes the treatment of arthrosis extremely effective. On average, the prosthesis lasts about 10 to 12 years, but there are cases of successful use with minimal wear and tear for 20 to 25 years.














































